Unveiling the Wonders of the Menstrual Cycle
Imagine your body as a finely tuned orchestra performing a unique symphony each month. The menstrual cycle is much like this concert: a harmonious sequence of events that prepares the body for a potential pregnancy. From the first day of bleeding marking a new cycle to the orchestrated interplay of hormones like estrogen, progesterone, FSH, and LH, every phase is vital. Starting at menarche between ages 10 and 15 and ending at menopause around age 50, this cycle is not just about biology—it’s a fascinating journey that impacts daily life in more ways than one.
Understanding the Menstrual Cycle
What is Menstruation?
Menstruation is the process where the uterus sheds its lining, leading to a flow of blood and tissue. This natural occurrence signals the start of a new cycle when an unfertilised ovum leads to the breakdown of the prepared uterine lining.
Key Milestones: Menarche and Menopause
Menarche: The onset of menstruation, usually between ages 10 to 15, marking the beginning of reproductive capability.
Menopause: The end of menstrual cycles, typically occurring between ages 45 and 55, signalling the conclusion of reproductive years.
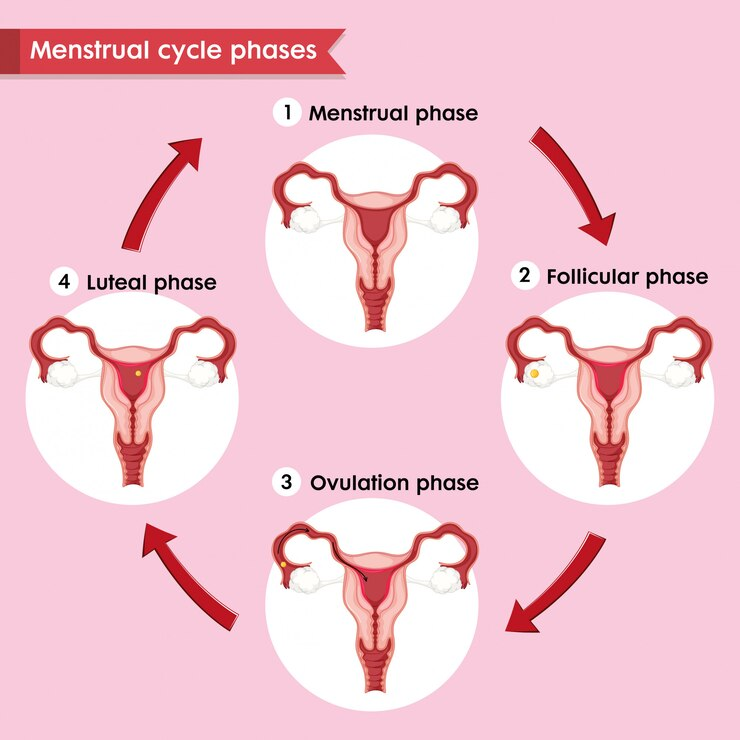
Phases of the Menstrual Cycle
The cycle is generally divided into four distinct phases:
Menstrual Phase:
Duration: Typically 3–5 days
Process: The uterus sheds its lining, resulting in menstrual bleeding.
Follicular Phase:
Duration: Follows immediately after menstruation
Process: Ovarian follicles develop, and the endometrium begins to rebuild in preparation for a potential pregnancy.
Ovulatory Phase:
Timing: Mid-cycle (approximately day 13–17)
Process: The mature Graafian follicle releases an ovum; this period is critical for fertilisation.
Luteal Phase:
Duration: Post-ovulation
Process: The corpus luteum forms and secretes progesterone to support the endometrium. In the absence of fertilisation, it regresses, triggering the next menstrual phase.
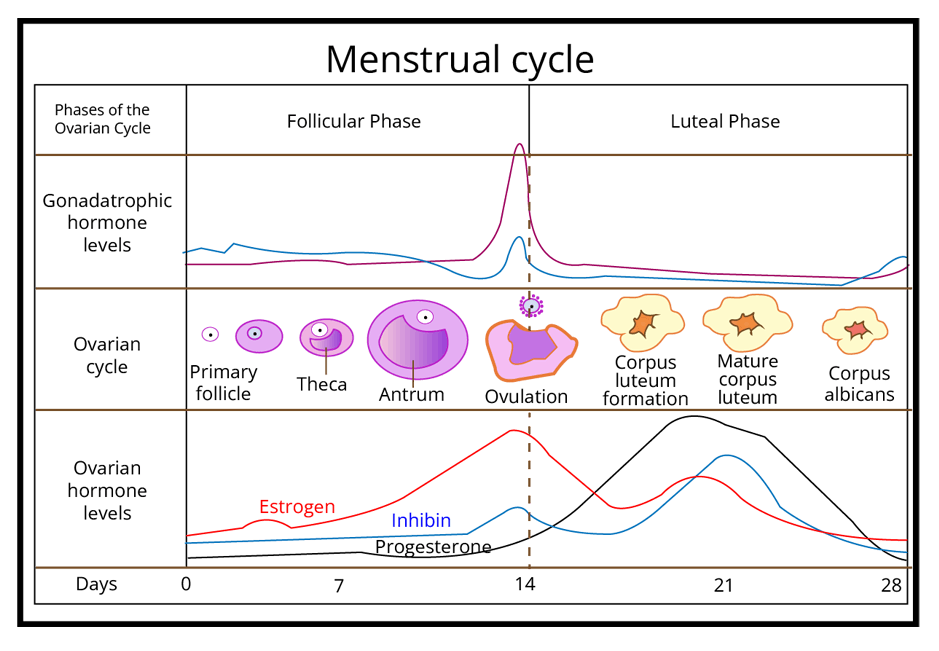
The Role of Hormones
Hormones are the body’s messengers that regulate the menstrual cycle. Here’s how they influence each phase:
FSH (Follicle-Stimulating Hormone): Stimulates the growth of ovarian follicles during the follicular phase.
LH (Luteinising Hormone): Peaks mid-cycle to trigger ovulation.
Estrogen: Promotes the thickening of the uterine lining.
Progesterone: Supports the endometrium after ovulation, preparing it for possible implantation.
For further exploration, you might consider reading related pages such as Oogenesis and Differences between Estrogen and Progesterone.
Quiz: How Well Do You Know the Menstrual Cycle?
1. What marks the first day of the menstrual cycle?
A) Ovulation
B) Menarche
C) The first day of menstrual bleeding
2. Which hormone is primarily responsible for triggering ovulation?
A) Progesterone
B) LH
C) Estrogen
3. What is the name given to the phase after ovulation?
A) Follicular phase
B) Luteal phase
C) Menstrual phase
4. At what age does menarche typically occur?
A) 10–15 years
B) 20–25 years
C) 5–8 years
5. What happens if the ovum is not fertilised?
A) Menopause occurs immediately
B) The corpus luteum secretes extra hormones
C) The uterine lining sheds, leading to menstruation
Check Your Answers:
C
B
B
A
C
Fun Facts About the Menstrual Cycle
Monthly Miracle: The menstrual cycle is nature’s way of preparing the body for pregnancy, occurring on average every 28–30 days.
Hormonal Dance: The delicate balance between estrogen and progesterone is crucial; even a slight imbalance can affect the cycle.
Global Variation: While many people experience a 28-day cycle, normal cycles can vary between 21 and 35 days, reflecting the natural diversity among individuals.
Real-World Applications
Understanding the menstrual cycle is essential beyond biology class. It helps in recognising patterns related to mood and energy, planning for school or work activities, and even guiding healthcare decisions. Additionally, knowledge about hormonal fluctuations can inform discussions about contraceptives and fertility planning, making it a vital part of overall health education.


FAQs on Menstrual Cycle: Phases, Hormones & Real-Life Insights
1. What is the menstrual cycle and what is its primary biological purpose?
The menstrual cycle is a series of natural changes in the female reproductive system that occurs monthly to prepare the body for a potential pregnancy. Its primary purpose involves the development and release of an egg (ovulation) and the preparation of the uterine lining (endometrium) to receive a fertilised egg. If pregnancy does not occur, the cycle concludes with the shedding of this lining, known as menstruation.
2. What are the four main phases of the menstrual cycle in their correct order?
The menstrual cycle is typically divided into four distinct phases that occur in a specific sequence:
- Menstrual Phase: The start of the cycle, where the uterine lining is shed, causing bleeding.
- Follicular Phase: Ovarian follicles mature, and the endometrium begins to regrow, driven by FSH.
- Ovulatory Phase: A mature egg is released from the ovary, triggered by a surge in LH.
- Luteal Phase: The corpus luteum forms and secretes progesterone to maintain the uterine lining.
3. Which key hormones regulate the menstrual cycle and what is the main function of each?
Four key hormones are responsible for regulating the events of the menstrual cycle:
- Follicle-Stimulating Hormone (FSH): Secreted by the pituitary gland, it stimulates the growth and maturation of ovarian follicles.
- Luteinising Hormone (LH): Also from the pituitary gland, a sharp increase (LH surge) triggers ovulation.
- Estrogen: Produced by the developing follicles, it causes the uterine lining to thicken and also influences pituitary hormone levels.
- Progesterone: Produced by the corpus luteum after ovulation, it maintains the thickened uterine lining, making it suitable for implantation.
4. How do pituitary hormones (FSH and LH) and ovarian hormones (estrogen and progesterone) interact to control the cycle?
The control of the menstrual cycle is a classic example of a hormonal feedback loop. The pituitary gland releases FSH and LH, which stimulate the ovaries. The growing ovarian follicles then produce estrogen. Initially, rising estrogen levels inhibit FSH production (negative feedback) but then cause a surge in LH (positive feedback), which triggers ovulation. After ovulation, the corpus luteum produces progesterone, which, along with estrogen, inhibits the pituitary from releasing FSH and LH, preventing new follicles from developing. If pregnancy doesn't occur, the drop in these hormones allows the pituitary to start releasing FSH again, beginning a new cycle.
5. What happens during the ovulatory phase, and why is the LH surge important?
The ovulatory phase is the shortest phase of the cycle, where the mature Graafian follicle ruptures and releases a secondary oocyte (ovum) into the fallopian tube. This event is critically dependent on the LH surge—a rapid and significant increase in Luteinising Hormone levels around day 14 of a 28-day cycle. This hormonal peak provides the final push needed for the follicle to rupture and release the egg, making it the most fertile period of the menstrual cycle.
6. What is the difference between the events happening in the ovary and the uterus during the menstrual cycle?
While interconnected, the events in the ovary and uterus are distinct. The ovarian cycle involves the development of follicles (follicular phase) and the formation and regression of the corpus luteum (luteal phase). In contrast, the uterine cycle refers to the changes in the endometrium, which include its breakdown and shedding (menstruation), its rebuilding (proliferative phase), and its preparation for implantation (secretory phase), directly responding to hormones produced by the ovary.
7. What is the significance of menarche and menopause in a female's reproductive life?
Menarche is the first menstrual cycle in a female's life, typically occurring during puberty. It signifies the beginning of the reproductive years and the capability to become pregnant. Menopause marks the natural and permanent cessation of menstrual cycles, which signals the end of a female's reproductive phase. It occurs due to the depletion of ovarian follicles and the subsequent decline in estrogen production.
8. How can understanding hormonal changes during the menstrual cycle help explain real-life variations in mood and energy?
Hormonal fluctuations have a direct impact on brain chemistry and can explain common real-life experiences. During the follicular phase, rising estrogen levels can boost mood and energy. Conversely, in the late luteal phase, a sharp drop in both estrogen and progesterone before menstruation can lead to premenstrual syndrome (PMS) symptoms, such as irritability, fatigue, and mood swings, providing a biological basis for these monthly patterns.
9. What happens to the corpus luteum if fertilisation occurs versus when it does not?
The fate of the corpus luteum is a critical branch-point in the cycle.
- If fertilisation does not occur: The corpus luteum degenerates after about 10-12 days. This causes a sharp decline in progesterone and estrogen levels, which triggers the shedding of the uterine lining (menstruation).
- If fertilisation occurs: The developing embryo produces a hormone called human chorionic gonadotropin (hCG), which 'rescues' the corpus luteum, causing it to continue producing progesterone. This progesterone is essential for maintaining the pregnancy until the placenta takes over.
10. Why can the length of a menstrual cycle vary from person to person and even month to month?
While an average cycle is 28 days, variation is normal and can be caused by several factors. The length of the follicular phase is the primary source of this variation. Factors influencing the cycle length include:
- Stress: High cortisol levels can interfere with reproductive hormones.
- Diet and Exercise: Significant changes can impact hormonal balance.
- Age: Cycles are often irregular after menarche and before menopause.
- Illness or medical conditions: Conditions like Polycystic Ovary Syndrome (PCOS) can cause irregularity.










