Discover the Intricacies of the Male Reproductive System
The male reproductive system is a marvel of biological engineering. In this guide, we explore the male reproductive system diagram, explain the structure of the male reproductive system parts, and delve into the function of male reproductive system. Our aim is to make these concepts easily understandable for students of all grades while offering unique insights that set our content apart.
Overview of the Male Reproductive System
The male reproductive system comprises various specialised organs that work together to produce, maintain, and transport sperm—the male gamete—and to synthesise male hormones. Unlike the female reproductive system, most male reproductive system parts lie outside the body, which is crucial for optimal sperm production.
Key Components Include:
Testes: Oval-shaped organs that produce testosterone and carry out spermatogenesis.
Scrotum: A sac that houses the testes and regulates their temperature.
Penis: The external organ with erectile tissues essential for intercourse and semen delivery.
Accessory ducts and glands: Including the rete testis, vasa efferentia, epididymis, vas deferens, seminal vesicles, prostate, and bulbourethral glands.
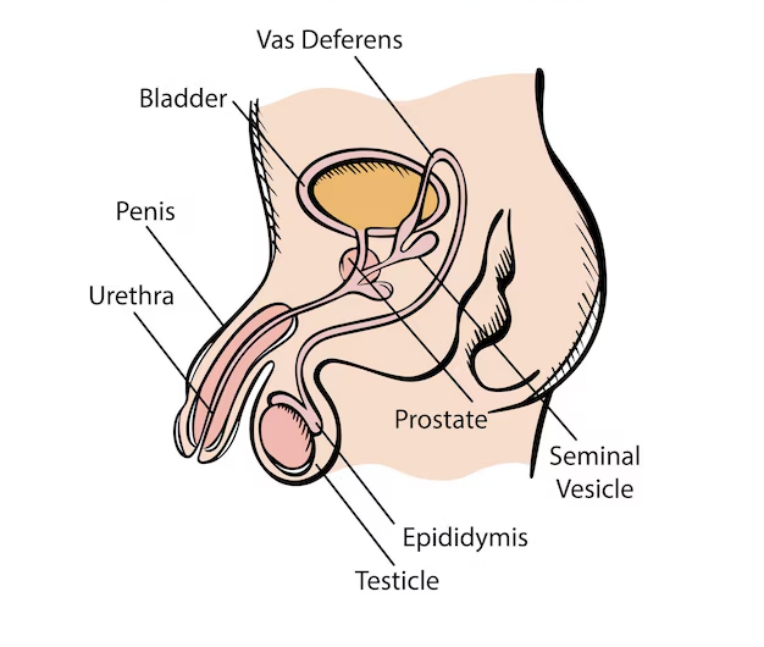
Male Reproductive System Diagram and Parts
A clear male reproductive system diagram helps visualise the anatomical arrangement and connectivity of its various parts. Let’s break down the components:
Testes: Each testis contains around 250 lobules where sperm production occurs in seminiferous tubules lined by spermatogonia (germ cells) and Sertoli cells. Leydig cells, found in the interstitial spaces, produce testosterone.
Accessory Ducts: Sperm travel from the seminiferous tubules to the rete testis, then to vasa efferentia, onward to the epididymis where they mature, and finally through the vas deferens towards the ejaculatory duct.
Penis and Urethra: The penis, made of erectile tissues (corpora cavernosa and corpus spongiosum), houses the urethra—a tube that serves dual roles in the reproductive and urinary systems.
Male Accessory Glands: Seminal vesicles, the prostate, and bulbourethral glands secrete seminal plasma. This fluid, rich in fructose, calcium, and enzymes, nourishes the sperm and makes up the bulk of semen.
Detailed Functions and Structures
Testes and Spermatogenesis
Structure: Oval bodies within the scrotum; each testis is subdivided into lobules.
Function: Production of testosterone and the process of spermatogenesis, ensuring genetic continuity.
Accessory Ducts
Structure: A network beginning with the rete testis, proceeding through vasa efferentia, epididymis, and vas deferens.
Function: Maturation, storage, and transport of sperm.
Penis and Urethra
Structure: Comprised of three types of erectile tissues and the urethra, which runs through the centre.
Function: Facilitates sexual intercourse and the expulsion of semen and urine.
Accessory Glands
Structure: Seminal vesicles, prostate, and bulbourethral glands are interconnected with the reproductive ducts.
Function: Secretion of seminal plasma, which enhances sperm viability and motility.
These explanations enhance our understanding of the structure of male reproductive system parts and clearly illustrate the function of male reproductive system.
Beyond the basics, it is important to appreciate the regulatory mechanisms and health aspects:
Hormonal Regulation: The hypothalamic-pituitary-gonadal axis plays a pivotal role in regulating testosterone production and spermatogenesis.
Temperature Control: The scrotum’s ability to contract or relax ensures that the testes are maintained at an optimal temperature, which is slightly lower than body temperature.
Health Considerations: Conditions such as varicocele, testicular torsion, and prostate enlargement can impact the normal functioning of the male reproductive system. Awareness and early diagnosis are crucial.
By integrating these unique details, we not only explain the male reproductive system parts but also offer insights into maintaining reproductive health.
Real-World Applications
Understanding the male reproductive system is vital for multiple real-life applications:
Medical Diagnostics: Knowledge of the structure of male reproductive system aids in diagnosing reproductive health issues.
Fertility Treatments: Insights into the function of male reproductive system are essential for addressing infertility.
Educational Tools: Detailed male reproductive system diagram illustrations serve as invaluable resources in biology education.
Public Health: Awareness programmes rely on accurate anatomical knowledge to promote healthy lifestyles and early intervention strategies.
Fun Facts About the Male Reproductive System
Temperature Sensitivity: The testes require a temperature slightly lower than the body’s core temperature, which is why they are housed in the scrotum.
Sperm Storage: Sperm mature and are stored in the epididymis, where they can remain viable for weeks before ejaculation.
Dual Role of the Urethra: In males, the urethra serves both the urinary and reproductive systems—a unique anatomical adaptation.


FAQs on Guide to the Male Reproductive System
1. What are the primary organs of the male reproductive system?
The male reproductive system consists of primary and secondary sex organs. The primary organs are a pair of testes. The secondary or accessory organs include the duct system (rete testis, vasa efferentia, epididymis, and vas deferens), accessory glands (seminal vesicles, prostate gland, and bulbourethral glands), and the external genitalia (penis and scrotum).
2. What are the two main functions of the testes?
The testes have two crucial functions as per the CBSE syllabus for 2025-26:
- Spermatogenesis: The production of male gametes, or sperm, within the seminiferous tubules.
- Hormone Production: The synthesis and secretion of the primary male sex hormone, testosterone, by the Leydig cells located in the interstitial spaces.
3. What is the complete pathway of sperm from the testes to the urethra?
The pathway of sperm begins in the seminiferous tubules of the testes where they are produced. From there, they travel through the following sequence:
- Rete testis
- Vasa efferentia
- Epididymis (where they mature and are stored)
- Vas deferens
- Ejaculatory duct (where it joins the duct from the seminal vesicle)
- Finally, into the urethra for expulsion from the body.
4. What are the components of seminal plasma and what role do the accessory glands play?
Seminal plasma is the fluid part of semen, produced by the male accessory glands. It nourishes and aids the transport of sperm. The contributions are:
- Seminal Vesicles: Secrete a fluid rich in fructose (energy for sperm), fibrinogen, and prostaglandins.
- Prostate Gland: Adds a milky, slightly acidic fluid containing citrate (a nutrient) and enzymes.
- Bulbourethral Glands: Secrete mucus that lubricates the penis before intercourse.
5. What are the key structures to identify in a diagram of the male reproductive system?
A standard diagram of the male reproductive system should clearly label the following key structures: the testis, scrotum, epididymis, vas deferens, seminal vesicle, prostate gland, bulbourethral gland, ejaculatory duct, urethra, and the penis. It is also important to show the path of the urinary bladder to illustrate the shared urinary and reproductive tract.
6. Why is the scrotum located outside the abdominal cavity?
The scrotum is located outside the abdominal cavity to maintain the temperature of the testes at 2–2.5°C lower than the normal internal body temperature. This lower temperature is absolutely essential for the process of spermatogenesis (sperm production), which cannot occur efficiently at the body's core temperature.
7. How do the hormones FSH and LH regulate the functioning of the testes?
The functioning of the testes is regulated by gonadotropins from the anterior pituitary gland.
- Luteinizing Hormone (LH): Acts on the Leydig cells (interstitial cells) and stimulates them to produce and secrete androgens, primarily testosterone.
- Follicle-Stimulating Hormone (FSH): Acts on the Sertoli cells and stimulates processes that support spermatogenesis, including the secretion of certain factors that help in the spermiogenesis process.
8. What is the difference between sperm and semen?
Sperm and semen are related but distinct. Sperm (or spermatozoa) are the microscopic, motile male gamete cells that carry genetic information. Semen is the composite fluid that is ejaculated, consisting of sperm mixed with the secretions from the accessory glands (seminal plasma). Essentially, sperm are the cells, and semen is the vehicle that carries and nourishes them.
9. What is the dual role of the urethra in the male body?
In males, the urethra serves a dual function for two different body systems. It is the terminal duct of the reproductive system, carrying semen from the ejaculatory ducts out of the body during ejaculation. It is also the terminal duct of the urinary system, carrying urine from the bladder out of the body during urination. A muscular sphincter prevents the two fluids from mixing.
10. Explain the significance of Sertoli cells and Leydig cells in spermatogenesis.
Sertoli and Leydig cells are two critical cell types within the testes that have distinct but complementary roles. Leydig cells, located in the space between seminiferous tubules, are responsible for producing testosterone, the hormone that drives male characteristics and spermatogenesis. Sertoli cells are located within the seminiferous tubules and provide structural support and nourishment to developing sperm cells, forming the blood-testis barrier and mediating the effects of FSH.










